Thyroid dysfunction and pregnancy
7-minute read
Key facts
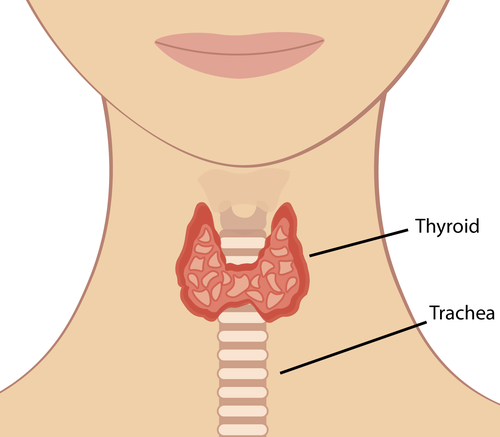
- The thyroid is a butterfly-shaped gland inside your neck that produces thyroid hormone.
- Thyroid hormone controls how your body uses energy (your metabolism) and is vital to maintain your health and your baby’s health during pregnancy.
- If you experience thyroid dysfunction during pregnancy, your thyroid becomes either underactive (hypothyroidism) or overactive (hyperthyroidism).
- Your doctor can detect unusual thyroid hormone levels with a blood test.
- If you have problems with your thyroid, your doctor may prescribe medicines to help.
What is the thyroid?
The thyroid is a butterfly-shaped gland inside your neck that produces thyroid hormone. This hormone controls how your body uses energy (your metabolism) and is vital to maintain your health. It is also important in supporting your and your baby's health during pregnancy.
Your thyroid problem may have started before your pregnancy. There are several types of thyroid dysfunction, including:
- Hypothyroidism: a condition where your thyroid gland produces too little thyroid hormone, causing a slowing down of bodily functions.
- Hyperthyroidism: a condition where your thyroid gland produces too much thyroid hormone, causing a speeding up of your bodily functions.
Other thyroid problems include thyroid nodules, which are abnormal growths or lumps in the thyroid gland that can affect how your body makes thyroid hormone, and thyroid cancer, which is a rare type of cancer that affects the thyroid gland.
How does pregnancy affect thyroid function?
Thyroid hormone levels increase during pregnancy to support you and your baby. While your baby’s own thyroid starts working in week 10 to 12 of pregnancy, it only fully matures in the third trimester. Until then, your baby relies on your supply of thyroid hormone for their brain development.
For this reason, it’s especially important that you have a healthy thyroid while you’re pregnant, for your own health as well as for your baby’s.
What is the difference between an overactive and an underactive thyroid?
During pregnancy, some people may experience thyroid dysfunction when their thyroid becomes either underactive or overactive.
An underactive thyroid (hypothyroidism), which can be due to:
- having too little iodine in your body
- a pre-existing immune disorder
- previous damage to the thyroid gland
An overactive thyroid (hyperthyroidism), which is usually a result of a condition that stimulates the thyroid gland too much, such as Graves disease.
Thyroid dysfunction affects 2 to 3 in every 100 pregnancies. If you have overactive or underactive thyroid dysfunction, your doctor will monitor you closely and recommend treatment specific to your situation.
What are the signs and symptoms of thyroid dysfunction?
Symptoms of an underactive thyroid include:
- very low energy levels
- feeling cold easily
- hair loss
- constipation
Some people may not notice any symptoms at all.
Symptoms of an overactive thyroid include:
- weight loss
- heat intolerance
- high blood pressure
What tests are used to check thyroid function?
Your doctor can detect unusual thyroid hormone levels with a blood test.
Regular screening is important if you have a higher risk of thyroid dysfunction, such as if you’re pregnant and have:
- symptoms of thyroid dysfunction
- a personal or family history of thyroid disease
- previous thyroid surgery
- goitre (swelling of the thyroid)
Regular screening is also recommended if you:
- have a history of miscarriage or premature birth
- have a history of infertility
- have type 1 diabetes
- live with overweight or obesity
- are aged 30 or older
If you fit into one or more of these categories, ask your doctor or midwife if your thyroid function should be checked.
How is thyroid dysfunction in pregnancy managed?
Underactive thyroid (hypothyroidism)
If you have hypothyroidism, your doctor may prescribe a medicine called thyroxine. Ideally, you should take these tablets before and after conception to optimise your thyroid hormone levels. You may also have your thyroid function checked regularly to ensure your thyroid hormone level is in the recommended range.
If left untreated, low levels of thyroid hormone can cause complications in pregnancy, such as premature birth, low birth weight and miscarriage. It may also affect the intellectual development of your baby.
Overactive thyroid (hyperthyroidism)
If you have hyperthyroidism, your doctor or specialist may prescribe medication to block thyroid hormone production (antithyroid therapy). The most common medicine used for this is called propylthiouracil.
If your thyroid gland is too active during your pregnancy, your baby has a higher than normal chance of having a higher heart rate (tachycardia), being born small (small gestational size), being born early (premature) or being stillborn.
What is the link between iodine deficiency and thyroid function in pregnancy?
Having too little iodine in your body is a common cause of low thyroid hormone levels. A study found that, on average, Australian females consume 100 micrograms of iodine a day. However, the World Health Organization recommends a daily intake of least 250 micrograms of iodine during pregnancy and breastfeeding.
Australian guidelines recommend that if you are pregnant or breastfeeding, you should take a supplement containing 150 micrograms of iodine each day (the amount found in most supplements).
Check with your antenatal health provider if you are concerned about your iodine levels, particularly if you are taking supplements such as pregnancy or pre-natal vitamins and minerals.
Your pharmacist will also be able to guide you on the potential impact of any prescription and over-the-counter medicines on iodine absorption and thyroid function.
Does thyroid function return to normal after the baby is born?
You will usually return to your regular thyroid function following the birth of your baby. However, after birth, 1 in 20 people may have ongoing irregular thyroid activity (postpartum thyroiditis). In some cases, your doctor may continue your thyroid hormone treatment until you have completed your final pregnancy. If you are taking medicines or supplements for thyroid dysfunction, check with your postnatal health provider after your baby is born. Be sure to let them know if you are breastfeeding or bottle feeding your baby, since this can affect your treatment.
Resources and support
If you are pregnant and have symptoms of an overactive or underactive thyroid gland, see your health provider and discuss your concerns.
Read the healthdirect page on Foods high in iodine.
Visit the Australian Thyroid Foundation for information, support and advocacy.

Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: January 2023





